What Does a Ruptured Disc Feel Like?
Introduction to Ruptured Discs
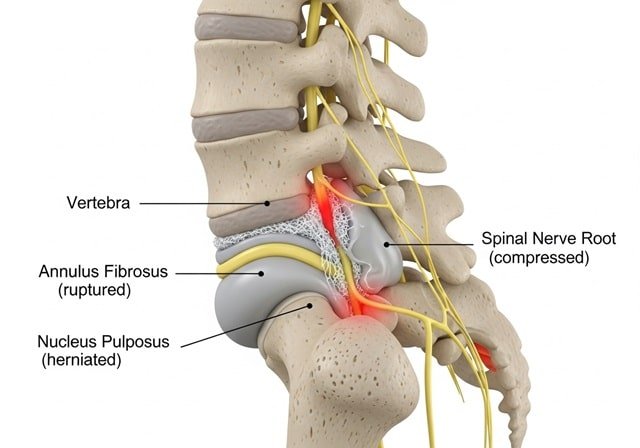
A ruptured disc, commonly referred to as a herniated disc, is a significant medical condition that can have profound effects on an individual’s mobility and quality of life. This condition occurs when the soft inner material of an intervertebral disc protrudes through a tear in the tougher exterior casing, which can place pressure on nearby nerves. Understanding the anatomy of the spine is essential to grasping how such a rupture transpires. The spine comprises several intervertebral discs, functioning as cushions between the vertebrae, enabling flexibility and pivotal support during movement.
Intervertebral discs are crucial for maintaining a healthy spine. They consist of a gel-like center called the nucleus pulposus encased in a stronger outer layer known as the annulus fibrosus. Various factors can contribute to a disc rupture, including age-related degeneration, excessive strain from physical activity, poor posture, and traumatic injuries. For instance, over time, the discs naturally lose hydration and elasticity, increasing the likelihood of a rupture from normal daily activities.
This condition is more prevalent among individuals aged 30 to 50 years, although anyone can be affected. Both genetic predisposition and environmental factors play a role in vulnerability to disc problems. The symptoms associated with a ruptured disc can range widely, influenced by the severity of the rupture and the specific nerves impacted. Common symptoms include persistent pain, numbness, and weakness, often manifesting in the legs or arms, providing a substantial insight into what does a ruptured disc feel like. By understanding these elements, individuals can better recognize the signs and seek timely medical intervention.
Common Symptoms Associated with a Ruptured Disc
Experiencing a ruptured disc can lead to a range of symptoms that may significantly impact daily activities. One of the most common symptoms is localized pain, which typically occurs in the area of the rupture. This pain can vary in intensity from a dull ache to sharp, debilitating anguish, making even simple movements challenging. For instance, an individual with a ruptured disc in the lumbar area may find it difficult to bend down or lift objects, affecting their ability to perform routine tasks such as gardening or cleaning.
Radiating pain is another prevalent symptom, often referred to as sciatica when it extends down the legs. This occurs when the ruptured disc compresses adjacent nerves, leading to a shooting pain that travels from the lower back through the buttocks and into the legs. Patients may describe this sensation as electric or like being struck with a jolt of pain, which can be aggravated by coughing or sneezing. Such symptoms can hinder mobility, restricting activities like walking or standing for extended periods.
Additionally, numbness and tingling sensations may accompany the pain. Individuals often report feeling a pins-and-needles sensation in their arms or legs, depending on the disc location. For example, those with cervical disc issues may experience these sensations in their shoulders and hands, leading to difficulties in grasping objects. These sensory disturbances can profoundly influence the quality of life, causing frustration and fear associated with loss of coordination or strength.
Overall, the symptoms associated with a ruptured disc vary by the location of the injury within the spinal column. Patients may encounter different combinations of pain, numbness, and tingling, depending on whether the rupture occurs in the cervical or lumbar regions. Understanding what does a ruptured disc feel like helps in recognizing these symptoms early for timely intervention.
Pain Experiences: Acute vs. Chronic
Understanding the pain experiences associated with a ruptured disc is essential for recognizing the condition’s impact on daily life. The two primary classifications of pain are acute and chronic, each representing distinct experiences and implications for the affected individual. Acute pain often arises suddenly, typically as a result of a specific injury or movement that aggravates the condition. This type of pain is characterized by its intensity, which can be debilitating and immobilizing. Patients may describe it as sharp, stabbing, or excruciating, often leading to an immediate need for medical attention. The sudden onset of a ruptured disc can catch individuals off guard, emphasizing the importance of immediate diagnosis and intervention.
On the other hand, chronic pain develops gradually, manifesting over an extended period, often persisting for months or even years. Unlike acute pain, chronic pain associated with a ruptured disc may begin as an intermittent discomfort that some individuals initially dismiss. Over time, this discomfort can evolve into a consistent, dull ache, which is frequently coupled with muscle weakness or numbness in the limbs. Chronic pain can be particularly challenging, as it often affects an individual’s emotional well-being, leading to feelings of frustration, anxiety, or depression. Personal anecdotes from patients reveal that living with chronic pain significantly impacts their daily activities, relationships, and overall quality of life.
In contrast to acute pain’s immediate severity, chronic pain often requires a multifaceted approach for management and relief. Various treatment options, including physical therapy, medication, and lifestyle changes, may be necessary to help alleviate symptoms. Understanding the differences between these two types of pain can better equip individuals experiencing the effects of a ruptured disc to seek appropriate care and support, improving their overall experience with this condition.
Impact on Daily Activities
A ruptured disc can profoundly affect an individual’s daily life, imposing limitations that hinder both physical and mental well-being. One of the most immediate consequences is the restriction in physical movements. Individuals frequently experience difficulties in bending, lifting, or even sitting for prolonged periods. These restrictions can emerge abruptly and might lead to significant discomfort, prompting a reevaluation of how one engages in routine activities.
The ability to perform regular tasks, such as grocery shopping, cleaning, or even engaging in hobbies, can be severely impacted. Whichever the context, the pain associated with a ruptured disc makes it arduous to enjoy activities that were once taken for granted. For instance, someone who enjoyed playing sports may find themselves sidelined, losing not only the physical activity but also the social aspect of participating with friends or teammates.
This condition can also impede work performance. Many professions require sustained physical activity or prolonged periods of sitting, both of which can exacerbate the discomfort from a ruptured disc. Consequently, individuals may need to adjust their working conditions, consider partial work leaves, or transition to less physically demanding roles. Coping strategies may include utilizing ergonomic furniture to support proper posture while sitting or taking frequent breaks to alleviate pressure on the spine.
Additionally, social activities may be curtailed, as individuals may shy away from gatherings that require traveling or prolonged standing. Adapting to these changes can be challenging; however, open communication with family and friends, alongside seeking professional advice on managing symptoms, can provide support during this difficult period. Understanding how a ruptured disc feels and affects daily life can be instrumental in finding effective coping strategies to navigate these challenges.
Diagnosis of a Ruptured Disc
Diagnosing a ruptured disc begins with a comprehensive assessment that includes a detailed medical history. Initially, the physician will inquire about the patient’s symptoms, including the nature and duration of pain, any radiating sensations, and the specific locations where discomfort is felt. This initial dialogue is critical, as it allows the doctor to develop a preliminary understanding of what a ruptured disc feels like in the context of the patient’s overall health.
A thorough physical examination follows this discussion. During this stage, the doctor will evaluate the patient’s posture, spine mobility, and muscle strength. Reflex tests may also be conducted to assess nerve function and identify any potential neurological deficits. These preliminary evaluations can help to narrow down the potential underlying causes of back pain, including the possibility of a ruptured disc.
To confirm a diagnosis of a ruptured disc, advanced imaging techniques are often employed. Magnetic Resonance Imaging (MRI) is the preferred method for visualizing disc integrity, as it provides detailed images of the spinal structures, including the discs and surrounding soft tissues. An MRI can reveal whether the disc has herniated or ruptured and assess the extent of any nerve involvement. In some cases, a Computed Tomography (CT) scan may also be utilized, particularly when MRI is not available or suitable for the patient.
Understanding the diagnostic process is essential for effective treatment planning. The combination of medical history, physical examination, and advanced imaging techniques plays a pivotal role in confirming a ruptured disc diagnosis. Proper identification of this condition ensures that appropriate therapeutic interventions can be implemented, addressing both the symptoms and their underlying causes. Effectively diagnosing what a ruptured disc feels like can make a considerable difference in a patient’s recovery journey.
Treatment Options for Ruptured Discs
Managing the discomfort and symptoms associated with a ruptured disc often involves a multi-faceted approach, encompassing both non-surgical and surgical treatment options. The specific treatment method usually depends on the severity of the condition and the intensity of the symptoms experienced by the patient.
Initially, conservative management is typically recommended for most individuals. This may include physical therapy, which helps strengthen the muscles that support the spine, thereby alleviating pressure from the affected area. Physical therapists often use tailored exercises that enhance flexibility and improve posture, which can substantially reduce the pain linked to a ruptured disc. Moreover, anti-inflammatory medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), are commonly prescribed to manage pain and decrease inflammation.
In some cases, steroid injections may be offered. These injections deliver corticosteroids directly to the area surrounding the impacted nerve root, providing significant relief from inflammation and pain. This approach can sometimes allow patients to return to their daily activities with minimal discomfort.
However, when conservative treatments fail to yield satisfactory results, surgical interventions may become a necessary consideration. One common surgical procedure for a ruptured disc is a discectomy, which involves the removal of the portion of the disc that is pressing on the nerve. Other options include laminectomy or spinal fusion, depending on the individual’s specific condition and symptoms. While these procedures can effectively alleviate pain and improve function, they do carry risks, including infection and nerve damage. Thus, a thorough discussion about potential benefits and complications with a healthcare provider is essential.
Ultimately, understanding the full spectrum of treatment options available for managing what a ruptured disc feels like is crucial for patients seeking relief. A collaborative approach between patient and healthcare team can lead to optimal outcomes and enhanced quality of life.
Lifestyle Adjustments and Management Strategies
Living with a ruptured disc requires significant adjustments to your daily routine to manage discomfort effectively. Understanding what does a ruptured disc feel like can guide individuals toward making necessary changes that alleviate symptoms and enhance quality of life. One critical area to focus on is ergonomics. Proper posture while sitting, whether at a desk or during leisure activities, can have a substantial impact on reducing strain on the spine. Individuals should ensure that their workspaces are set up to support their back health, using chairs that provide lumbar support and positioning computer screens at eye level to avoid slouching.
Incorporating gentle exercises into your routine can also be beneficial. Physical activity is essential for strengthening muscles that support the spine and can provide relief from the intense sensations associated with a ruptured disc. Activities such as swimming, walking, or yoga specifically tailored for back pain can promote flexibility and strength. However, it is crucial to seek professional advice from a healthcare provider or physical therapist before beginning any new exercise regimen to ensure safety and effectiveness.
Additionally, modifications in daily routines may contribute to an improved lifestyle. This can include taking frequent breaks during long periods of sitting or standing, as well as using supportive braces during activities that may exacerbate discomfort. Techniques such as lifting heavy objects correctly—by bending the knees instead of the waist—are vital to prevent further injury. Understanding what does a ruptured disc feel like is essential in identifying activities that should be minimized or avoided altogether.
Ultimately, making these lifestyle adjustments and management strategies can significantly aid individuals experiencing the challenges of a ruptured disc. Prioritizing comfort, safety, and flexibility while being attentive to the body’s signals is essential in navigating daily life with this condition.
When to Seek Medical Attention
Recognizing the signs and symptoms associated with a ruptured disc is critical for ensuring timely medical intervention. While some symptoms may be manageable, certain warning signs require immediate evaluation by a healthcare professional. It is essential to be aware of these indicators to facilitate an accurate diagnosis and effective treatment.
One alarming symptom that signifies the urgency of seeking medical help is the loss of bladder or bowel control. This condition might suggest that the ruptured disc is compressing the spinal nerves responsible for regulating these functions. Such a situation often indicates a medical emergency, as it may lead to permanent nerve damage if not addressed promptly.
Another red flag is severe weakness in the legs. This symptom can manifest as difficulty standing, walking, or even maintaining balance. When a ruptured disc presses on specific nerve roots, it can lead to significant motor deficits. If weakness progresses or starts affecting both legs simultaneously, immediate medical attention is paramount to prevent further complications.
Additionally, any progressive symptoms that seem to worsen over time should not be overlooked. This includes increasing pain levels, numbness, or tingling in various regions of the body. If these symptoms intensify or begin to affect daily activities, it is essential to consult a healthcare provider. Early intervention is crucial, as it can drastically improve recovery outcomes and may prevent surgical interventions.
In essence, knowing what does a ruptured disc feel like and recognizing its warning signs can empower individuals to seek timely medical advice. Understanding when to act can make a significant difference in the prognosis and quality of life following a ruptured disc diagnosis.
Conclusion and Encouragement for Those Affected
Experiencing a ruptured disc can significantly impact one’s quality of life, leading to various symptoms such as pain, numbness, and physical limitations. As discussed, the sensations associated with a ruptured disc may vary widely among individuals. Some report sharp, radiating pain while others experience chronic discomfort and weakness. Understanding what a ruptured disc feels like is crucial for anyone dealing with this condition, as it provides a framework to recognize symptoms and seek timely medical advice.
It is essential for individuals afflicted by a ruptured disc to remain proactive in their health journey. Engaging with healthcare professionals should be a priority, as they can offer personalized diagnosis and treatment options tailored to the severity of the condition. Ignoring the symptoms or delaying consultation may lead to further complications. Therefore, recognizing the signs and seeking help is a vital step towards recovery. Regular check-ups and keeping an open line of communication with medical providers can assist in effectively managing symptoms.
Secondly, hope and positivity play a crucial role in recovery from a ruptured disc. While some may experience debilitating effects, advancements in medical interventions have promised improved outcomes. It is beneficial for individuals to stay informed about their condition, exploring various treatment modalities, including physical therapy, medication, and possibly surgical options when necessary. Community support can also be invaluable; finding local or online support networks where individuals share experiences may provide emotional buoyancy and practical advice for coping with the challenges presented by a ruptured disc.
In conclusion, understanding what a ruptured disc feels like empowers those affected to navigate their health proactively. The importance of consulting healthcare providers, remaining hopeful, and leveraging support systems cannot be overstated. This multifaceted approach can significantly enhance the journey towards recovery and improved wellbeing for those individuals facing this ailment.